-
PDF
- Split View
-
Views
-
Cite
Cite
Usama Boles, Ibrahim Almuntaser, Angie Brown, Ross R.T. Murphy, Azra Mahmud, John Feely, Ventricular Activation Time as a Marker for Diastolic Dysfunction in Early Hypertension, American Journal of Hypertension, Volume 23, Issue 7, July 2010, Pages 781–785, https://doi.org/10.1038/ajh.2010.58
Close - Share Icon Share
Abstract
A standard 12-lead electrocardiogram (ECG) is performed in all hypertensive patients, primarily to detect left ventricular hypertrophy. Echocardiographic assessment of hypertensive subjects reveals that abnormalities in diastolic function occur more commonly and earlier than increased left ventricular mass. However, ECG changes associated with diastolic dysfunction (DD) remain poorly defined; we assessed the ventricular activation time (VAT) (i.e., the time for the ventricle to depolarize) as a potential marker for DD in early hypertension.
Ninety subjects (aged 46 ± 1.3 years; 43 men) with newly diagnosed, untreated hypertension underwent ECG and comprehensive two-dimensional echocardiography. Left ventricular DD was echocardiographically assessed using Canadian Consensus Guidelines. We compared VAT, which corresponds to the QR interval in the 12-lead ECG, with echocardiographic parameters of DD.
VAT was prolonged in subjects with DD (46.3 ± 0.4 vs. 39.6 ± 0.3 ms, P < 0.01). There was a significant correlation between VAT and tissue Doppler imaging (TDI) (early diastolic velocity) e′ (r = −0.53, P < 0.0001), (ratio of early and late diastolic velocities) e′/a′ (r = −0.53, P < 0.0001), transmitral Doppler (TMD) (early peak filling rate, and early deceleration peak) E/A (r = −0.32, P = 0.001), and (ratio of early diastolic mitral inflow and early diastolic velocities) E/e′ (r = 0.44, P < 0.0001).
Prolongation of the VAT is associated with DD in patients with newly diagnosed untreated hypertension.
Hypertension is one of the commonest chronic conditions in the developed world, present in 30–40% of the adult population.1 Complications of poorly controlled hypertension may lead to cardiac functional and structural changes resulting in heart failure.2 Reports suggest that diastolic dysfunction (DD) in the left ventricle (LV) occur early in the course of hypertension and may precede detectable LV hypertrophy (LVH).3,4 Furthermore, the standard 12-lead electrocardiogram (ECG) is commonly normal in hypertension and LVH is seen in only 10–20% of patients. A 12-lead ECG is standard for the assessment of all hypertensive patients.5,6 Early diagnosis of DD is crucial and ECG criteria may be of clinical value.
Atrial changes may occur in DD and may be associated with P wave abnormalities. These abnormalities have been studied in DD patients, but measurement difficulties and low sensitivity in identifying either the cause or severity of the DD are obstacles that make it impractical in the clinical situation.7 As early as 1982, the close relationship between the delay in the time for the ventricle to depolarize (VAT) (also known as intrinsic deflection) and left atrial (LA) abnormalities were documented in spontaneous hypertensive rat models.8 However, we know little about similar changes in humans. In humans, VAT can be estimated from the ECG by measuring from the onset of the QRS complex to the peak of the R wave (QR interval).
VAT in V5 or V6 of >0.05 s is used as one of the Romhilt-Estes9 scoring criteria for diagnosing LVH. However, the extent to which VAT is affected by DD in patients without LVH is unknown. We therefore compared VAT in the ECGs of newly diagnosed hypertensive patients with and without DD against echocardiographic findings.
Methods
We prospectively examined 90 subjects with newly diagnosed untreated hypertensive. Subjects (48 women; mean age 46 ± 1.3) had (three readings >140/90mmHg and an ambulatory daytime BP 135/85mmHg). Those with evidence of heart failure (symptoms or signs), ischemic heart disease, arrhythmia, diabetes, abnormal renal function, secondary causes of hypertension, or valvular heart disease or receiving hemodynamically active drug therapy were excluded. The study was performed in accordance with the declaration of Helsinki, the patients gave informed consent and the study had institutional ethics committee approval.
Blood pressure was measured in the right arm in the supine position by an observer blind to therapy using an oscillometric device (Omron, model HEM 705-CP, Omron, Tokyo, Japan) in triplicate and the mean was used for further analysis.
A 12-lead high resolution ECG (GE, MAC 5000, New York) was taken at rest, with 1mV/cm amplitude and 25mm/s rate. Standard ECG with clear QR duration was sought in all study cohort. We enlarged the ECG using a scanner and Adobe Photoshop software. Measurements were calibrated on underlying standard ECG graph paper. VAT was measured in ms in the 12 leads and was defined as the average measurement from the onset of the Q wave to the peak of the R wave (QR interval). The measurements from V6 were compared with the mean value calculated from 12 leads. The beginning of the P wave was defined as the point where the initial deflection of the P wave crossed the isoelectric line, and the end of the P wave was defined as the point where the final deflection of the P wave crossed the isoelectric line. P wave dispersion was calculated by subtracting the minimum P wave duration from the maximum P wave duration. ECG criteria (by Cornell voltage-duration product and/or Sokolow–Lyon voltage), was used for diagnosing left ventricular hypertrophy.10
Echocardiographic assessment was made using a commercially available ultrasound system (Sonos 5500, Philips, Andover, MA) equipped with Doppler tissue echocardiography capabilities. Baseline echocardiography examinations were done to rule out structural abnormalities. Cardiac dimensions were calculated using standard M Mode.11 Left ventricular mass index (LVMI) was measured based on American Society of Echocardiography's guidelines.12 Left ventricular hypertrophy was considered present when the LVMI exceeded 115g/m2 (male) or 95g/m2 (female).12,13 LV DD was defined using the criteria provided by the Canadian Consensus guidelines14,15 using transmitral Doppler (TMD) with and without the Valsalva maneuver. TMD of the peak early E wave (peak early diastolic velocity) in cm/s, peak late A wave (peak late diastolic velocity) and cm/s, their ratio (E/A), E wave deceleration time, and isovolumic relaxation time were recorded. The same measurements were repeated during phase II of the Valsalva maneuver. Tissue Doppler diastolic velocities were measured from the septal, lateral, inferior, and anterior mitral annuli in the 2- and 4-chamber views and averaged. The following measurements were recorded: early diastolic velocity (e′) and late diastolic velocity (a′) and their ratio (e′/a′). The ratio of early diastolic mitral inflow velocity (E) to tissue Doppler imaging (TDI) e′ (E/e′), which correlates with diastolic filling pressure,14 was considered. Two blinded independent operators recorded the ECG and echocardiographic data.
Statistical analysis. Analysis was done by JMPIN statistical software, version 5.0 (SAS for Windows). Results are expressed as mean ± s.e.m., P < 0.05 was considered significant. Differences between means were analyzed using analysis of variance and Wilcoxon rank sum tests were used. Relationship between clinical parameters was analyzed using Spearman Rho correlation analysis. The determinants of VAT in assessing of diastolic function was analyzed using stepwise multiple regression analysis with age, gender, LA dimension, LV mass index, interventricular septal diameter, TMD E/A, TDI e′, e′/a′, and E/e′ as covariates.
Results
We classified our cohort of 90 patients into two groups according to the absence (N = 40) or presence (N = 50) of DD based on echocardiography parameters. There were no differences between the two groups in age, gender, height, weight, body mass index, waist circumference, systolic or diastolic BP (Table 1).
Baseline characteristic of 90 newly diagnosed untreated hypertensive patients
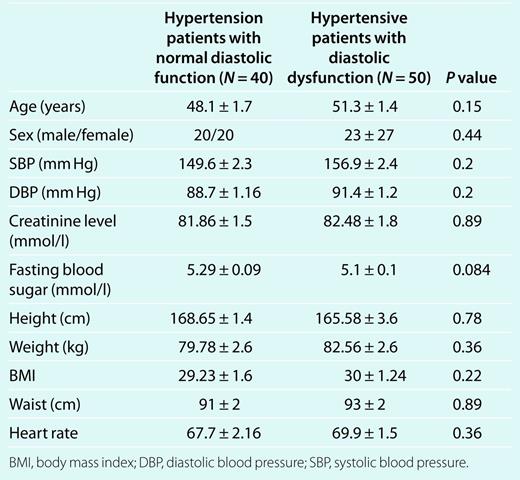
Baseline characteristic of 90 newly diagnosed untreated hypertensive patients
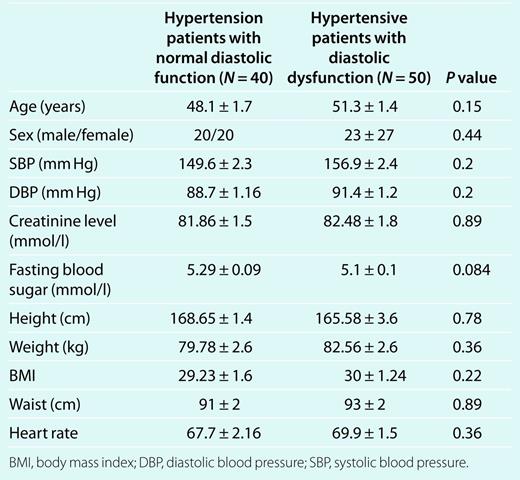
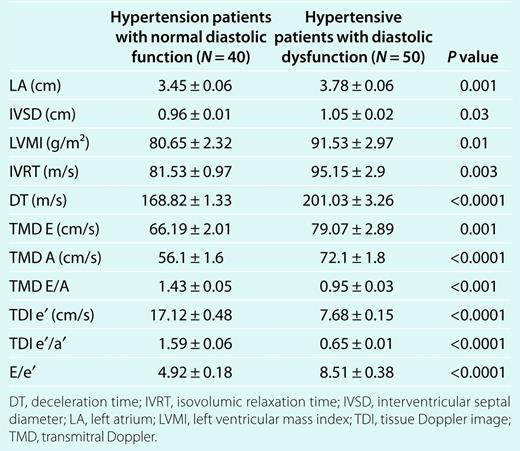
Table 2 showed that, subjects with DD had a higher LA diameter (P < 0.01), interventricular septal diameter (P = 0.03), LVMI (P = 0.01), and E/e′ (P < 0.0001) and a lower TDI e′, and e′/a′ (P < 0.0001). Although LA diameter increased from 3.4 ± 0.06cm in normal to 3.8 ± 0.06cm (P = 0.001) in the DD group, prevalence of dilated LA diameter in subjects with DD was 25% in women with cutoff 3.8cm and 14% in men with cutoff 4.2cm.
Echocardiography parameters in subjects with diastolic dysfunction and subjects with normal diastole
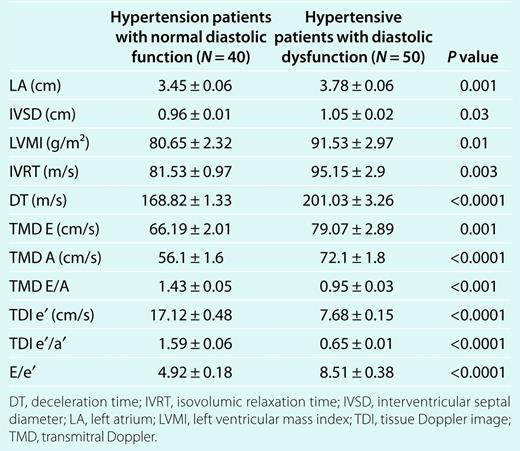
Echocardiography parameters in subjects with diastolic dysfunction and subjects with normal diastole
There were no significant interobserver variations in LVMI measurement (r = 0.93; P < 0.0001). Based on American Society of Echocardiography's guidelines (LVMI exceeded 115g/m2 (male) or 95g/m2 (female)), there were 16 (32%), out of 50 with DD, have LVH.15,16 However, there was no evidence of LVH was recorded according to ECG criteria. LVMI was higher when corrected for height and body mass index in DD group (P = 0.01).
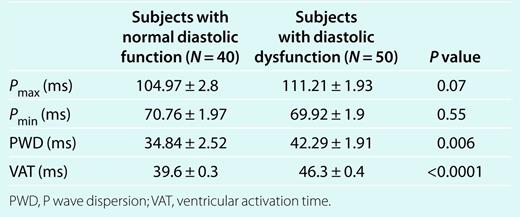
Interestingly, VAT increased with DD, from 39.6 ± 0.3 in subjects with normal diastolic function to 46.3 ± 0.4 in subjects with DD (P < 0.0001) (Table 3 and Figure 1).There were no significant interobserver variations in VAT measurements that the two consecutive measurements were significantly related to each other (r = 0.90; P ≤ 0.0001). There was no significant difference between VAT measured in 12 leads and in V5 or V6 (r = 0.86, 0.90; P < 0.001). VAT correlated with LV mass index and LA diameter (r = 0.27, 0.25; P = 0.01) but not with relative wall thickness. VAT also correlated inversely with TMD E/A (R = −0.32, P = 0.001), TDI e′ (r = −0.61, P < 0.0001) (Figure 2), and TDI e′/a′ (r = −0.5, P < 0.0001) and positively with E/e′, which estimates LA pressure (r = 0.44, P < 0.0001). There was a significant increase in P wave dispersion from 34.84 ± 2.52 in normal subjects to 42.29 ± 1.91 (P = 0.006) in the DD group. However, there was no significant correlation of P wave dispersion with echo parameters.
Electrocardiography parameters in subjects with and without diastolic dysfunction
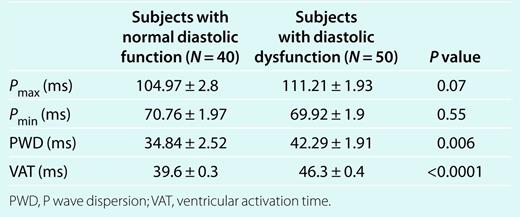
Electrocardiography parameters in subjects with and without diastolic dysfunction
The ventricular activation time (VAT) in subjects with normal diastolic function and diastolic dysfunction.
Relationship between ventricular activation time (VAT) and e′ tissue Doppler imaging (TDI).
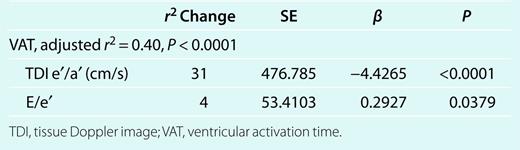
In stepwise regression model (Table 4), tissue Doppler e′/a′ and E/e′ were the only independent determinants of VAT in assessing DD with no contribution from age, gender, LA dimension, LV mass index, interventricular septal diameter, TMD E/A, TDI e′, as covariates (r2 = 0.40; P < 0.0001).
Data for the covariates and their coefficients, 95%, CI in stepwise regression analysis
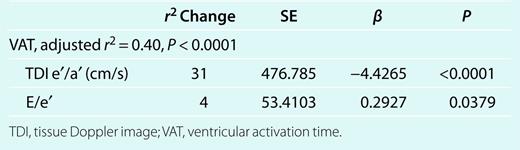
Data for the covariates and their coefficients, 95%, CI in stepwise regression analysis
Discussion
Reports in late 1980s and early 1990s suggested that DD occurs early in the course of hypertension and precede measurable LVH. This study focused on a hitherto neglected area of standard 12-lead ECG changes associated with diastolic abnormalities in early hypertension. Although the new guidelines put an emphasis on the early echocardiographic changes in heart failure, however, myocardial remodeling may occur early before any detectable damage. Electrical remodeling may happen even earlier in the course of the disease.17 VAT may increase as a result of electrical remodeling, with LVH patients, even if LVM was unchanged.18 In our study, we hypothesized that VAT may prolong in subjects with DD and normal LVM.
Although electrical asynchrony and prolongation of VAT has been shown previously in patients with asymmetric myocardial changes,19 therefore in our study, we measured VAT in the 12 leads initially for accurateness. Yet, V6 readings gave matching results with the mean value of VAT in 12 leads; it could be used in the future—for simplicity—in clinical practice.
Previous studies have concentrated on changes in P wave morphology and duration, reflecting LA pressure changes occurring with DD,9,20 we found statistical differences in PWD in our cohort between both groups. Similarly, VAT (which reflects early ventricular depolarization) was increased in subjects with DD and was also significantly related to DD parameters detected by TDI and TMD studies.
It has been argued that transmitral velocities in TMD studies are influenced by pressure preload whereas that TDI values are far less affected by it.21,22 If so, the strong negative relationship between VAT and the TDI parameters such as e′ and e′/a′ support our hypothesis that a prolongation of VAT is an independent marker of DD in patients with hypertension.
Moreover, VAT increased with E/e′, a ratio that estimates LV filling pressure, an indicator of diastolic filling abnormalities,22 thus providing further evidence of a relationship between VAT and DD.
Interestingly, in our cohort, a dilated LA diameter by gender-specific cutoffs was seen in only 14% of men and 25% of women. Although LA volume index would be a better parameter, it was not measured in our cohort. Obvious LA dilatation is more likely to occur later in the course of the disease, when LVH has already developed.23
We have documented prolonged VAT in patients with early hypertension and echocardiographic evidence of DD. VAT has not previously been studied in DD in early hypertensive patients. Further studies in a variety of settings are now required to determine the sensitivity and specificity of prolonged VAT as a valid ECG marker for DD.
Our cohort was all patients with newly diagnosed hypertension and was categorized based on the presence or absence of DD with no normal subjects enrolled in the study. Another limitation found in our bias of selecting subjects with evidence of DD. The reason for that we sought it may give more comprehensive idea about VAT changes if studied in large cohort with diastolic abnormalities. Finally, left ventricular strain and LA volume index were not assessed by echocardiography study. We believe the latter may be of importance to our study.
Disclosure
The authors declared no conflict of interest.
References
1.
2.
3.
4.
5.
6.
7.
8.
9.
10.
11.
12.
13.
14.
15.
16.
17.
18.
19.
20.
21.
22.
23.


